Encephalitis is a heterogeneous group of disorders including both infectious encephalitis and Autoimmune Encephalitis (AE). Encephalitis is a common neurological disease and a major public health concern in the United States with more than 20,000 hospitalizations per year and a fatal outcome in 5.8 percent. It is estimated that over 50 percent of patients remain without a clear diagnosis and etiology (or cause) despite an extensive work up. However, recent research shows that autoimmune encephalitis is not as uncommon as previously thought. One study, found an incident rate (from 1995-2015) of autoimmune encephalitis was 0.8 per 100,000 people (1).
Particularly in younger patients, less than the age of 30 years old, autoimmune encephalitis is found more frequently than viral encephalitis (2). Forms of autoimmune encephalitis include paraneoplastic disorders, classically associated with cancer, and other antibody-mediated diseases associated with cell-surface antibodies that may or may not be associated with cancer.
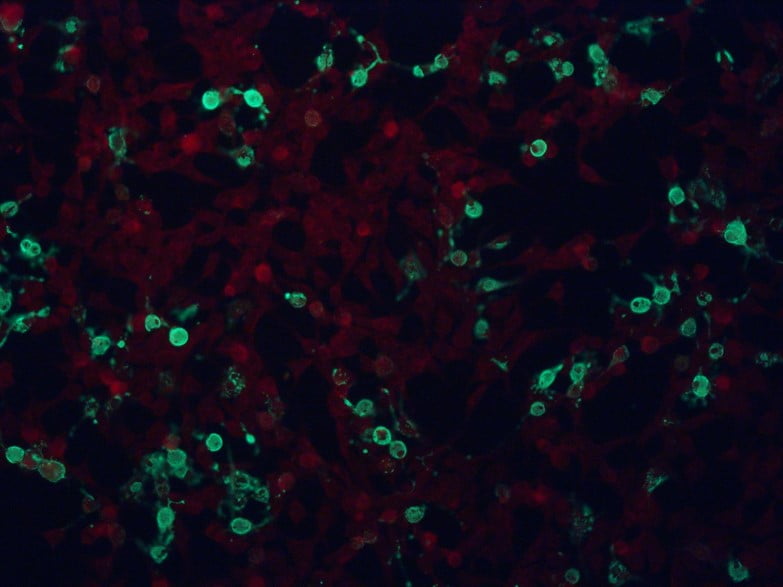
The diagnosis of autoimmune encephalitis is based on the overall clinical picture and looking various parts of the diagnostic work up. Sometimes a clear antibody is found, but many times an antibody is not found. As our understanding of autoimmune encephalitis grows, we will likely continue to discover new antibodies since these auto-antibodies continue to be discovered at a very rapid pace. Additionally, there are limitations to antibody testing and not all the antibodies we recognize to cause autoimmune encephalitis are commercially available for testing yet.
The discovery of new neural autoantibodies has revealed that these conditions are much more common than previously appreciated and often times patients are misdiagnosed or remain undiagnosed. As the increased awareness of autoimmune neurological disease continues to increase, it is likely more patients will be diagnosed and will require appropriate treatment.
The two most common antibody-mediate autoimmune encephalitides are NMDA receptor encephalitis and LGI1 autoimmune encephalitis which are detailed here:
NMDA receptor encephalitis
What is NMDA receptor encephalitis?
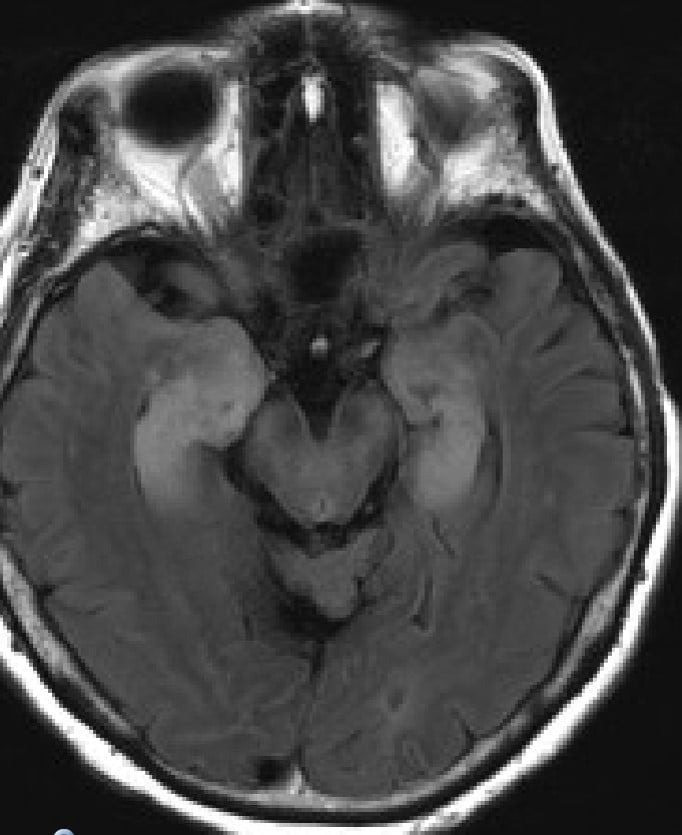
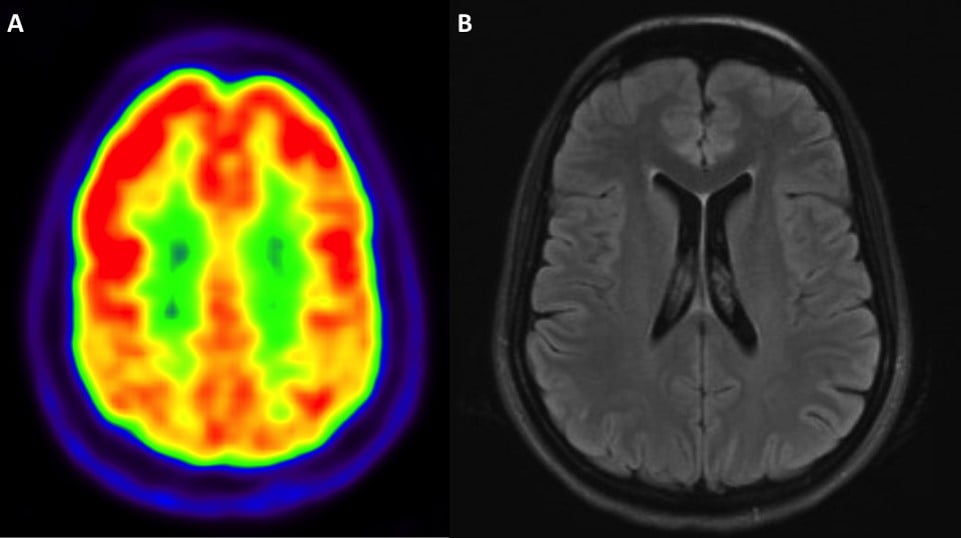
Anti-NMDA receptor encephalitis was first described in 2007 as a syndrome of memory problems and confusion, psychiatric symptoms, seizures, hallucinations and movement disorders in four young women with ovarian teratomas (3). Since that time, there have been many causes reported in children, as well as, young to middle age adults including men and women without an underlying tumor. This syndrome is often diagnosed based on the presentation of rapid onset of abnormal or psychiatric behavior, speech dysfunction, seizures, abnormal movements, decreased level of consciousness and/or autonomic dysfunction. Diagnostic testing often includes a lumbar puncture, brain imaging (MRI), and electroencephalogram (EEG). Patients often have evidence of inflammation in their CSF and the diagnosis is confirmed when patients are found to have a positive NMDA receptor antibody in the CSF.
Neuroimmunology Nuggets: Anti-NMDA-R Encephalitis
What are the symptoms?
Anti-NMDA receptor encephalitis patients may have a flu-like illness before the onset of psychosis, hallucinations, memory problems and many times seizure and abnormal movements. Untreated, patients can eventually develop respiratory failure and coma. Overall patients typically respond well to immunotherapy and should be treated rapidly. Sometimes, depending on severity, it can take a longtime to slowly recover.
What are the treatment options?
Immunosuppressive therapies used in the treatment of anti-NMDA receptor encephalitis. First-line therapies include intravenous steroids, intravenous immunoglobulin (IVIg), or plasma exchange. Second-line therapies often include off use label of rituximab and/or cyclophosphamide.
Rapid diagnosis and early treatment is essential in the treatment of autoimmune neurological disease, particularly in the setting of cell-surface antibody-mediated encephalitis such as NMDA receptor encephalitis. Treatment approaches are largely based on expert opinion and retrospective studies currently, as there is a strong need for future research with prospective trials (4). There are no randomized, prospective clinical trials in the treatment of anti-NMDA receptor autoimmune encephalitis currently.
LGI1 autoimmune encephalitis
What is LGI1 autoimmune encephalitis?
LGI1 autoimmune encephalitis is a rare antibody-mediated autoimmune encephalitis (5). It is likely to be the second most common form of antibody-mediated autoimmune encephalitis after NMDA receptor encephalitis. It often causes a limbic encephalitis which is an inflammatory process of the limbic system and temporal lobe of the brain which is a vital part involved in forming memories and emotions. Individuals with this condition have severe short-term memory problems and often seizures with characteristic changes of inflammation in the temporal lobes seen on the brain MRI. Some individuals develop a distinct seizure pattern called faciobrachial dystonic seizures either before or at the onset of the limbic encephalitis and can provide a clue to the diagnosis.
What are the treatment options?
Similar to Anti-NMDA receptor encephalitis, immunosuppressive therapies used in the treatment of LGI autoimmune encephalitis. There are no randomized, prospective clinical trials in the treatment of LGI autoimmune encephalitis.
Neuroimmunology Nuggets: LGI1 Encephalitis
Autoimmune Epilepsy
What is Autoimmune Epilepsy?
Autoimmune epilepsy can be caused by the same class of antibodies seen in encephalitis, however seizures predominate the clinical presentation. Often seizures come on rapidly and are severe and refractory to standard anti-seizure medications (6) (7).
What are the treatment options?
Treatment approaches are similar to autoimmune encephalitis with the use of immune therapies. First-line therapies include intravenous steroids, intravenous immunoglobulin (IVIg), or plasma exchange. Second-line therapies often include off use label of rituximab, mycophenolate mofetil, or azathioprine. Again, there are no randomized, prospective clinical trials in the treatment of autoimmune epilepsy.