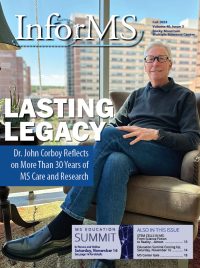
Preparing for his retirement after more than three decades in the field, the MS Center’s Dr. John Corboy reflects on his career and shares his hope for the future of MS care.
In this issue, we’re looking back at the career of Dr. John Corboy, who’s wrapping up his remarkable tenure with his impending retirement from clinical care in October of 2024. Dr. Corboy has touched countless lives through his more than three decades serving people and their families living with MS in Colorado and beyond.
Dr. Corboy is the Medical Director of the Rocky Mountain MS Center nonprofit organization, as well as Director of the Rocky Mountain MS Center at University of Colorado (RMMSC at CU).
Corboy was the founder of the University of Colorado MS Center (UCMSC) in 1997, also launching the first MS Clinic at Denver Health and resurrecting neurological MS care at the Rocky Mountain Regional VA Medical Center. The UCMSC began the development of a comprehensive, patient-centered care model for treating MS that would serve as the foundation for today’s Rocky Mountain MS Center.
We recently sat down with Dr. Corboy to explore his career, the progress he’s seen in more than 30 years of MS care, and what he hopes the future holds for his patients and the field of MS treatment, care and research.
InforMS: What drew you to the field of multiple sclerosis in the first place? Can you give us a synopsis of your early career and the decisions that led you to where you ended up in medical school and beyond?
John Corboy: In my misguided youth, I thought it’d be a great idea to get a PhD in Anthropology. So after college at University of Pennsylvania, I entered a PhD program to study physical anthropology, which looked at the evolution of biological and behavioral human traits. I was especially interested in evolution of the brain as it related to behavior.
But I realized shortly after being there that although it was extremely interesting, there was no easy or good path forward in becoming an anthropologist. My mother had always wanted me to be a doctor, so I decided to apply to Medical School instead. I had to actually go back to do my Pre-Med work because I hadn’t done that as an Anthropology undergraduate major.
I had the good fortune of going to the University of Pennsylvania Medical School, which had a very strong Neurology department. The first day I walked onto my required Neurology rotation, one of the godfathers of Neurology, Arthur Asbury, happened to be my attending physician. For a month I spent time with Dr. Arthur Asbury — that’s what really helped convince me that Neurology was a field that suited my skills and interests. My brain sort of thought the way neurologists thought.
They had two parts of the program that were very strong. One was neurovirology. In those days, oftentimes the people who studied neurovirology in the laboratory were MS doctors, because there was a strong feeling and some data to support the idea that MS was related in some way to viruses. So people who were virus people in labs often saw MS patients in clinic.
But in addition, the MS group was just very strong there. My senior year of residency, I spent the entire year working with Dr. Francisco Gonzalez-Scarano, who later went on to become the chair of neurology at UT San Antonio. He was one of those people who was a neurovirologist but saw MS patients in clinic. The way we were structured, you were assigned to one faculty member for the entire year. So I was in clinic with him for an entire year.
That got me much more interested in MS, because I saw the kinds of linkages that might be related to virology and neurologic diseases, especially those that were not obviously virological diseases like MS. So it was kind of a natural progression when I finished my residency that I would want to stay in those two broad fields. My fellowship was at Johns Hopkins in neurovirology.
But there was a quirk — I thought I was going to do my one half-day a week of clinic in the HIV clinic, because that’s what I was studying in the lab. But in fact, they had way too many people already working the HIV clinic, and someone had left the MS program. A couple hundred MS patients that needed to be taken care of, and there was no one available to see them. So they said, “Why don’t you see them, John?” That’s in fact exactly what happened.
InforMS: How has MS care evolved over the years that you’ve been practicing?
Corboy: Broadly, I can tell you essentially what my fellowship was like — it ended in 1992, and the first disease modifying therapy (DMT) was in approved 1993, which was interferon beta-1B, or Betaseron.
 In my fellowship, I worked in the lab nine half-days a week, and one half-day a week I went to the clinic. There was a nurse practitioner there, and we just saw whoever was there. That was it, that was my fellowship.
In my fellowship, I worked in the lab nine half-days a week, and one half-day a week I went to the clinic. There was a nurse practitioner there, and we just saw whoever was there. That was it, that was my fellowship.
What was at our disposal in the late 1980’s? Well, we could see them and examine them. We could make sure the diagnosis was correct by the standards of the day, and that was before the more formal diagnostic criteria had developed.
Just leading up to that I had the good fortune of training during a time when MRIs became available. In addition, sadly but importantly, the HIV epidemic occurred. Immunology was somewhat of a backwater prior to the development of more sophisticated immunological drugs and before HIV. Perhaps one of the positive things that came out of the HIV epidemic was a greater understanding of all the intricate portions of the immune system. The impact that had on autoimmune diseases was incredible. It went from somewhat of a backwater from the scientific point of view to near top of the table. What happened primarily is that people like me got interested in immunology.
This also had a huge impact on the development of a rational approach to clinical trials. There had been clinical trials previously in MS but they were very naïve and not well planned by today’s standards. But you had to start somewhere, and that’s where they started.
For example, when it became clear that MS was likely related, at least in great part, to autoimmune system dysfunction, they started saying, “Well, maybe we should just try to suppress the immune system.” But the studies were not sophisticated enough as yet to be able to look at specific populations of MS patients. There wasn’t a good understanding that the disease evolved over time, and that a person who was 70 was not the same as a person who was 30 with regard to their autoimmune dysfunction. So many of the original trials failed.
As I was finishing fellowship in 1992, that was the time when more rational studies (by today’s standards) tried to parcel out which subpopulations might be most amenable to the available therapeutic options.
All of those original studies for the early drugs that got approved were done in restricted populations, restricted by age and type of MS. That revolution was all taking place. MRIs, a new understanding of immunology and a more rational approach as to how we would try to identify populations of people that would benefit potentially — all of that was occurring at the same time.
So when I came out of fellowship, our arsenal consisted of making the best diagnosis available, confirming the diagnosis, and when someone had an acute attack we would use steroids very similar to what we use today still. The plasma exchange studies had not been done yet, so we didn’t have plasma exchange as a second use after steroid failure.
“We could treat spasticity with baclofen. We could treat pain like trigeminal neuralgia with tegretol. We had canes, wheelchairs, physical therapy, prayer, and not a whole heck of a lot else. That’s what it looked like when I took my first job at the University of Minnesota in 1992.” — Dr. John Corboy
The change that occurred was remarkable and dramatic. But even still it took a while.
There’s a concept in medicine called therapeutic inertia, where it takes a long time for new discoveries to actually get implemented into clinic. When Betaseron became available, what became very clear was that both the doctors and the patients were reluctant to start using the drug.
Once the idea that we could actually alter the natural history of MS became embedded, probably over three or four years, things really evolved dramatically, and our whole discussion of how we interacted with people changed completely. Now, all of a sudden front and center was something that might alter the natural history of the disease. Nobody was so naive to believe that this was somehow magical and a cure for MS. But at the same time, it offered MS patients a dramatic level of hope that didn’t previously exist. That was a sea change in terms of how we think about treating MS.
If you’d asked people during my time of training what would the evolution look like, no one would have put MS at the top of the list or anywhere near the top of list of conditions for which we would have significant treatment impacts in the near term.
I actually gave a talk to medical students once on the concept of what neurology was at that point in time, and the title of the talk was “The End of Diagnose and Adios.” The prior concept was you’d go see a neurologist, get a diagnosis, then just go back to your primary care physician because they couldn’t do anything. This was the beginning of the end of that.
InforMS: Can you take us through the next 10 years or 15 years after that point?
Corboy: There were different phases that we went through. The first phase was that therapeutic inertia, which was very brief thankfully, but was present. Then we had three or four drugs, and they just got traded around. That is, if you failed one, you would simply try another. People would literally bounce from one to another because they were modestly effective, and many people failed them either because they had new disease activity, or did not tolerate them. And of course we didn’t know what level of disease activity was significant enough to count as a failure. Some people counted it as a failure if you got one new dot on your brain scan. At the same time some people would say, “Well, you can have three or four attacks over three or four years, and that’s okay.”
We didn’t even have an understanding of what to expect from the drugs. But they ping-ponged around, and sometimes people would go from one interferon to another.
So that was Part A of the DMT era. Everything changed when Tysabri got approved. In 2004, at the American Academy of Neurology meeting, the actual data became available pretty much during the meeting. On the spot, they created an entire session just for the Tysabri data and put it in the largest room they had available. Literally about 2,000 people crammed into a room to hear this. There was a buzz about it that was going on already, and it was clear that this was going to be a change.
Tysabri had been on the market for two months when I gave a talk about Tysabri to the Colorado Society of Neurology. Quite a few people had started to use it because the whole concept had changed — we went from no treatments to modest treatments and then to a modern biological, IV drug that was clearly superior. The very last part of my talk was about known safety issues, which were modest. But I cautioned that we needed much more information and time to judge the safety.
Then, just one month after my talk, the drug was taken off the market because of the first three cases of the severe brain infection, progressive multifocal leukoencephalopathy, or PML, including one in Colorado. It remained off the market from February 2005 until July 2006, so over a year, almost a year and a half, before it came back. This experience changed things several ways:
Number one, it showed we could potentially approach MS with a much more specific, targeted therapeutic, because this drug really targeted a specific molecule.
And two, it demonstrated that we can harm people significantly with these treatments. That was really a paradigm shift as well. People got sick with flu-like side effects from the earlier drugs, and rarely someone would have to stop them due to liver enzyme elevations. But severe, life-changing adverse events were rare and manageable. Now this drug comes on the market and is taken off literally 90 days later.
That’s when we entered the modern era of understanding the nature of risks and benefits, and the need to manage these.
I would say from 2006, when it came back on the market, to today — so that’s 18 years — has really been the more modern era.
But the targeting that has occurred, first with Tysabri and then more recently with many drugs, including the CD20 drugs like Ocrevus and others, has changed dramatically.
“The nature of our understanding of the immune system and the targeting that’s taken place has evolved significantly. All the drugs going forward are likely going to be very targeted.” — Dr. John Corboy
As the variation in effectiveness and risk of the DMTs evolved, so has how we use the medications. For at least 10 years, there had been an argument about how we use them, how we stage them, how we sequence them. Should we use highly effective therapy early? Or should we continue to start with the older, better-known DMTs, and only escalate to the more highly effective drugs if the drugs fail?
Although that argument isn’t completely settled, I think it’s changed dramatically from what it was 10 years ago. My partner, Tim Vollmer, would have these debates in public at meetings with a couple thousand people present. He would get up and argue logically and passionately for more highly effective therapy early. At the end of the day, 10 years ago, when the discussion was over, people would vote, and they would vote for escalation, not high-efficacy therapy early.
If you did that today, that would no longer be the case. We now have numerous head-to-head trials showing overtly that outcomes are better when you use more highly effective therapy early. Our whole team should be proud that we were early leaders in the movement towards early, high-effectiveness therapy. [Editor’s note: Dr. Corboy and Dr. Vollmer served together as Co-Directors of the Rocky Mountain MS Center at CU from 2008 to 2021.]
But with this comes risk that needs to be managed. We are presently undergoing the next great change: defining limits to the medications as people age and use the drugs for prolonged periods of time. That’s where the DISCOMS and de-escalation studies come in, which recognize that we have to understand MS as a condition that changes with aging and what may be great at 30 may be less necessary, or even more risky, when you are 60.
When you use rituximab, for example, a drug that was originally designed to treat people with cancer for a year or two before they either died or were cured, we’re now using it for 10 or 15 years. How do those usages change? What are the risks? They change dramatically.
InforMS: Where do you think things are headed now?
Corboy: Now the focus, I think, is appropriately shifting, to looking beyond just manipulating the immune system.
That’s where remyelination, neuro-protection and regeneration comes in.
If you ask people today what the most important question is in terms of altering the natural history of the disease, I would hope they would say: How do we stop the death of partially damaged cells, and how do we repair them? Ultimately, how do we reverse damage to the brain and spine that has already occurred?
Because at this point, we’ve manipulated the immune system extensively and gotten significant benefit out of that. But we’ve now found the limitations associated with that approach.
When I talk to patients, I tell them I’ve never been more hopeful in my entire life with regard to the potential for medicine to help with this condition specifically.
With regard to potentially regenerating nervous tissue, we’ve gone from it being considered crazy talk, to then science fiction, and now to science. The pace of change is extraordinary. I am reminded of the movie Contagion from 2011 about a pandemic that started in China. In that movie, they go from all these people dying — looking a lot like our recent pandemic — to isolating the virus, developing a vaccine, and putting it in people’s arms in a year.
I was watching that movie when it first came out and said, “You know, I’m trained in virology, and this is just not realistic.” And yet the COVID-19 pandemic happened, and that’s exactly what happened. We had a vaccine in under a year.
So why should we not think something like that’s possible for MS as well?
InforMS: Can you speak about the power of advocacy, both from an organizational standpoint, and what individuals can do?
Corboy: Advocacy is incredibly important. It’s often the last thing on the list of things to do, but in many respects, it can have perhaps the most powerful impact. It requires constant attention and unrelenting pressure to get what is best for our patients. Advocacy is important at multiple levels, with professional organizations playing a very large role, but patients also play a crucial part.
For example, we go to the Pharmacy and Therapeutics Committee with Colorado Medicaid every January. This committee decides how Medicaid will cover the available drugs, which is a huge challenge given the high costs of many medications, not just for MS but also for conditions like cancer and hepatitis C.
At these meetings, there’s a large presence of pharmaceutical companies, each getting about three minutes to make their case. However, I can tell you that the people who get listened to the most are nonprofits like us and the patients themselves.
When I went in front of the committee once, I gave my three-minute presentation and then answered questions for 45 minutes. No pharmaceutical representative got that kind of attention. The committee sees us every year, they know us, and when we speak honestly about what’s important and how things work functionally in the office, they listen.
A concrete example of this was when Ampyra (dalfampridine) came on the market. It was a relatively expensive drug, and Medicaid was trying to figure out how to use it. Some insurances tried to put limits on its use, requiring documentation of at least a 25% improvement in walking ability after a year to continue coverage.
We explained that patients use this drug for various reasons, not just for walking. It might help people using wheelchairs maintain the ability to feed themselves or manage personal hygienic care. We asked them to remove the clause about taking away coverage if walking speed didn’t improve by 25%, and instead to allow documentation of any clear benefit to the patient. They changed the rule based on our input.
This is just one example of how patient experience and our persistence in advocacy can have an important impact. Subsequently, studies have shown that dalfampridine can be helpful for various symptoms, not just walking speed.
Another significant change coming in January 2025 is that insurance companies will no longer be able to “double-dip” by charging deductible payments from both the individual and whoever is assisting them in paying for deductibles and copays. We were involved in advocating for this change at the local level, and when attempts were made to claw back some of that progress this year, we fought back again, and it never made it out of legislative committee.
 There’s no substitute for this kind of persistent pressure to advocate for people with MS and other conditions. Patient stories play a big role in this. Patients are people, just like legislators and those working for insurance companies and pharmaceutical firms. They have a right to speak up and say how policies impact them and why they think things should change.
There’s no substitute for this kind of persistent pressure to advocate for people with MS and other conditions. Patient stories play a big role in this. Patients are people, just like legislators and those working for insurance companies and pharmaceutical firms. They have a right to speak up and say how policies impact them and why they think things should change.
The combination of patient stories, the persistence of our organization, and aligned organizations can be very powerful in effecting change.
InforMS: Is there anything today that surprises you?
Corboy: Maybe not surprising, but humbling, is the seat that we have as physicians, as we help people navigate this mysterious set of conditions that are remarkably variable and change so suddenly. To watch people deal with all of these challenges and retain their hopes and dreams, have their families, and live their lives to fulfillment, is extraordinary.
Regarding the science of what we do, the pace of change seems to be ramping up. For example, when I trained, we learned that the cells needed to regenerate nervous tissue did not exist in the nervous system, Now, in the space of no more than 15-20 years, we have gone from not only knowing these cells exist, but to actively manipulating them in the first attempts to repair cells inside human beings. This is a profound change in our understanding of the biology of the nervous system. When I came out of residency in 1989, that was the biggest difference from today. Now we think of the nervous system as a dynamic, changing part of our human organism.
I’ll be out of med school 40 years next May, and to me, that’s the biggest change. The other significant developments I mentioned before are in terms of understanding the immune system and how imaging can change our perspective. Imaging, in many respects, has completely altered our view of what we think multiple sclerosis is.
Another profound development is our understanding of the cross-talk between different conditions and systems, not just within the nervous system, but within the entire body. How our immune system intersects with our nervous system is very important. This understanding was pretty naive when I first started training.
The changes in the basic and clinical science are really what keeps people coming back and going to work every day, I think. For me, that has been perhaps the most humbling thing in my career —
I’ve been able to work in a field where I get up and every day I learn something new.
InforMS: What gives you the most hope for the future of MS?
Corboy: What I see on the whole, in spite of whatever cynicism exists in medicine and among some of the public, is that organized medicine — from professional organizations to individual physicians, and now with all the other providers that we have helping us — the vast majority really do wake up in the morning and go to work wanting to try and help people. And from the patients, they respect these efforts and really do want to be part of the solution for themselves and for others. That is why they are willing to literally put their bodies on the line to enter clinical trials.
Fundamentally, I think the approach we have in terms of using science to try and help people, that is not broken. And that is really a good thing.
That, I think, hasn’t changed, and that’s what gives me hope.
The Rocky Mountain MS Center invites you to celebrate Dr. Corboy’s dedication to the care and treatment of MS, his commitment to his patients, and his service to our community with a donation to the Dr. John Corboy Legacy Fund. Learn more and donate by visiting MSCenter.org/Corboy.