Fatigue is not only one of the most common MS symptoms, it’s also one of the most frustrating for people to manage. In this issue, we’re presenting an update to a past article written by Patricia Daily, LCSW. There have been studies and other developments over the years, but much of what we know (and still don’t know) about fatigue simply hasn’t changed. We hope this information helps you better understand MS fatigue, learn about different tools that can help manage it, and helps friends and family understand the intensity and overwhelming nature of this troubling symptom.
Fatigue is the most common MS symptom and, in competition with pain, is the most frustrating for people to manage. It is unpredictable and invisible and is often misattributed, not to the MS disease process, but to depression, denial, disinterest, self-pity, disorganization, poor planning or just plain laziness. As many as 80 to 90 percent of people with MS have fatigue, and probably half of them experience it every day. One third of people with MS describe it as their most troublesome symptom. Fatigue is a frequent cause of disability.
Fatigue is difficult to define because it is a collection of different symptoms that vary in frequency and intensity. Although fatigue is a big problem, it is a slightly different problem for each person who has it, so it is difficult to measure and therefore difficult to study.
We will explore MS fatigue – what it is, what causes it, and most important, what you might do to manage it.
Fatigue: What is it?
 Fatigue is an imprecise term. It is meant to describe tiredness that is out of proportion to the effort exerted, occurs suddenly and unpredictably, and significantly interferes with the necessary functions of everyday life.
Fatigue is an imprecise term. It is meant to describe tiredness that is out of proportion to the effort exerted, occurs suddenly and unpredictably, and significantly interferes with the necessary functions of everyday life.
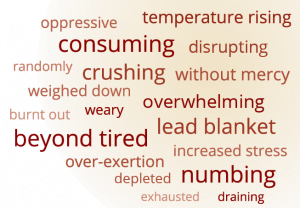
Because it has many facets, fatigue is difficult to define and it is very difficult to describe to people who don’t have it. We use standard vocabulary words such as tired, exhausted, and worn out to describe it, but “tired” does not do justice to the subjective experience of MS fatigue. The feeling of “tired” is familiar to everyone on the planet. In normal life, we use “tired” as a way to describe how much energy we have expended, but it does not describe how much energy we have left. “Tired” is how we feel after we clean the garage, read a long and dull report, or exercise for an hour. Our energy is diminished and we would prefer to rest, but if circumstances demand it, we can override tired, tap into our reserves and carry on.
Fatigue is tired that cannot be overridden. When people are fatigued, they have run out of energy to the point where rest or sleep is essential. Their reserves are exhausted and they cannot muscle their way through.
Dimensions of Fatigue
Fatigue can be loosely classified according to dimensions such as fatigue type, severity, frequency and the amount of disruption it causes.
Physical fatigue causes a decrease in endurance that is out of proportion to the circumstance that provoked it. People who experience it seems to run out of gas sooner than expected based on their level of health and fitness. Someone might experience increasing physical tiredness during a short walk and begin to show symptoms, for example poor coordination or foot drop. The problem can usually be improved with a brief rest, after which some energy returns and the symptoms subside. People new to MS often try to push through physical fatigue but without success. It is similar to a cell phone that won’t hold a charge – you can talk until the battery runs down but then you have to stop. When the battery is recharged, you can talk again, but you have to take time to recharge the battery.
Cognitive fatigue diminishes mental stamina and makes it difficult to focus attention. It is as if the “muscle” that supports attention and concentration just gives out. People report that they “can’t think,” lose track of what they are doing, and are more likely to make mistakes, even when doing a familiar task. This type of fatigue is often worse in the afternoon.
Lassitude is a general tiredness and is described as a global lack of energy. It can appear as a lessened capacity for work, reduced efficiency, usually accompanied by feelings of weariness, sleepiness or irritability. Some experience excessive sleepiness. One woman with MS describes it as “hitting the wall. I simply shut down. Then I don’t care. It doesn’t matter what I am doing. I have to stop.” Others describe an absence of motivation to do anything that requires effort. Most people need to rest and about half report that they have to sleep. Most find rest or sleep to be restorative.
The distinction between fatigue “types” is not crisp and there is lots of overlap. It is common for people to have more than one manifestation of fatigue.
Another dimension of fatigue is its severity. Some people have mild fatigue but some have severe fatigue that prevents them from working. Fatigue severity can also be temporarily intensified by other factors, such as a demanding and stressful life event or a brief illness. The majority of people report that heat and humidity increase their fatigue.
Frequency is another factor in fatigue. For many people, fatigue is a daily occurrence. It often has a waxing and waning pattern. It is minimal in the morning, most evident by early afternoon and often subsides in the evening. Sometimes it develops gradually, but sometimes the onset is quite sudden and surprising. Sudden and severe fatigue can be the first sign of an exacerbation. Fatigue can be provoked by circumstances. A very busy and demanding day may result in an accumulation of fatigue that carries into the following few days. People can accumulate a tiredness debt, if they overdo it, and it can take a few days to pay it off. But many times people experience fatigue for no reason whatsoever and this can be perplexing and frustrating. “How can I possibly be this tired? I didn’t do anything.” It can also be discouraging – “Am I ever going to get this right?” and embarrassing – “I feel like a big wimp.”
There is also variability in the amount of disruption MS fatigue causes for a person. For example unpredictable fatigue that is less severe can be more disruptive than severe fatigue that happens every day and requires a 3 hour nap, because you can plan for the latter.
The presence and severity of fatigue does not appear to be related to sex, disease duration, or age. It is not determined by the degree of physical disability or the number of MRI lesions. Several studies report a strong connection between disease severity and fatigue. However, people with what might appear to be “mild” MS can have really severe fatigue and some people with progressive MS have no fatigue at all.
Causes of Fatigue
What causes fatigue is not well understood. It appears to be primarily caused by the MS disease process. However, it is influenced by an array of other factors such as general health, activity level, heat, humidity, and sleep, as well as personality, mood and coping style. Fatigue occurs in other autoimmune disorders, but MS fatigue is unique because it is worsened by heat.
Imagine that MS fatigue is a spring-fed lake, also filled by a bunch of little creeks that flow into it. The primary source of water is the spring, but the little creeks also contribute. The more that any of these sources flow into it, the fuller the lake becomes. The MS disease process is the primary source of fatigue. Secondary factors are those other sources that feed into and intensify fatigue.
Primary Fatigue
There are different theories about what creates primary fatigue, and some thought that the different types of fatigue have different underlying processes.
One hypothesis is that MS related fatigue is caused by ongoing inflammation. There is evidence that alterations in the immune system alter the level of cytokines which are thought to be strong mediators of fatigue.
Another theory is that fatigue comes about because the brain is damaged. The MS disease process causes demyelination and axonal injury. Although the brain can recover from this and rewire itself, it simply takes more energy to get around the damaged areas. The brain has to recruit more areas and work harder to compensate for the damage. That extra energy expenditure results in fatigue.
It can be helpful to think of your brain as a kind of network – like a highway system in a metropolitan area. Imagine that you’re driving from your home to your office 10 miles away. If there are no accidents or heavy traffic, it will be smooth sailing. But if road construction is underway, traffic is terrible, and you need to take a detour, it’s a different story. You’ll still get to your office, but you’re going to use more gas and you’re going to get there later. If the connections in your brain aren’t flowing smoothly, you can still get things done, but it’s going to take more energy and it might take more time.
Another hypothesis is that fatigue is somehow related to a general reduced level of activity in certain parts of the brain. People who experience fatigue show a 10-20 percent reduction in glucose metabolism in areas of the brain that control important cognitive functions including memory and in other areas that affect movement. The metabolism of glucose provides fuel for the brain, so fatigue may result from a diminished fuel supply.
We also know that there are lesion locations in the brain that are more associated with fatigue. For example, there are areas in the brain stem that can control the level of alertness. If you have an MS lesion in one of those spots, your level of alertness can be lowered. If you have a lesion in one of your motor tracks – the fibers that come from brains and go to your limbs – you’re not only going to have weakness, but it can cause increased fatigability from physical exertion.
Secondary Sources of Fatigue
There are many other factors that contribute to fatigue. Some are related to MS, but many are common to all of us. A really big cause of fatigue is life on earth, with all its relationships, noise, demands, and complexities. Children, spouses, pets, and politicians all add to the mix. Just being alive and busy is a source of fatigue.
Some medications that are used to treat MS symptoms such as pain, spasticity, or bladder overactivity can be sedating and contribute to fatigue.
Mobility impairments that make it more difficult for someone to get around can contribute to fatigue because it simply takes more energy and is therefore more exhausting to get places. Environmental obstacles, for example stairs, can use up a lot of energy. Heat increases fatigue. So does humidity.
Being out of shape can cause fatigue. People with MS tend to be less physically active. Chronically reduced activity can result in deconditioning, and this can cause increased fatigability.
Other medical problems can contribute to fatigue. Thyroid dysfunction, anemia, renal and hepatic insufficiency, vitamin D deficiency, and infections can all contribute to fatigue.
Sleep disturbance, depression, stress, and pain frequently show up in MS and can play a significant role in fatigue. Each of these can also be an independent cause of fatigue. They all appear to be related to each other and — similar to that gang of surly kids that haunted the halls of middle school — have a tendency to be more troublesome when they hang out together.
Not surprisingly, sleep disturbance appears to be a good predictor of fatigue and is significantly related to depression. Studies suggest that there is “an intimate but complex” relationship between MS fatigue and sleep. People with MS are twice as likely to have reduced sleep quality as healthy people without MS. When clinicians evaluate fatigue in an individual patient, one of the first issues they explore are potential sleep disorders. Primary sleep disorders include insomnia, sleep apnea, periodic leg movements in sleep, or REM sleep disorders. Identifying and treating these disorders can improve sleep and lessen fatigue.
Depression is a complicated issue in MS. The incidence of major depression is five times greater in MS than in the non-MS population and is believed to be a primary symptom of the disease. Elevated pro-inflammatory cytokines are implicated in MS exacerbations, fatigue, depression and stress. Treatment of depression in MS has been shown to decrease the production of pro-inflammatory cytokines and to reduce fatigue.
The behavioral aspects of depression also play a role in fatigue. Reduced self-efficacy – the sense that you have no control – is a predictor of physical, cognitive and global fatigue. Reduced self-efficacy and a tendency to over-focus on symptoms are both common in depression and also appear to aggravate fatigue. Stress is also a predictor of mental fatigue. Changes in mood – for example, increased optimism – appear to diminish the perception of general fatigue severity.
Pain is also a common problem in MS, and as anyone who has had it can attest, pain can be exhausting. It can also disrupt sleep, which can contribute to depression and limit physical activity, which can in turn contribute to deconditioning, and both of these can contribute to fatigue.
Treating Fatigue
Clearly, there are multiple factors that contribute to fatigue. How they work and how they might interact with each other isn’t understood. When people talk about “overwhelming fatigue” in MS they certainly refer to the magnitude of the tiredness and energy loss. But “overwhelming” also describes the complexity of the problem. Treating MS fatigue is very complicated. Figuring out what to do about it all can be overwhelming. Where do you start?
It isn’t true that there are no good treatments for MS fatigue. It is true that there is no single, easy-to-find and simple-to-do treatment. There are ways to improve MS fatigue, but just as the symptom is not straight forward, neither are the solutions. Most MS fatigue is caused by a combination of factors that each contribute a bit to the development of fatigue. The solution, therefore, is likely to be a combination of little changes that create gradual improvement.
There are two types of interventions to manage fatigue. There are medications and there are other, mostly behavioral, interventions such as sleep, cooling, energy conservation strategies, exercise, and cognitive behavioral therapy.
Treatment Adherence
It is important to adhere to your disease modifying therapy (DMT) in order to help prevent exacerbations and to prevent or lessen the brain atrophy. Taking your DMT helps to prevent your MS from getting worse, and also calms the inflammation that we think plays a role in fatigue.
Medications
There are no FDA approved treatments for MS fatigue. Some medications are used off-label to treat fatigue. They have all been studied in various clinical trials and the results have been mixed, but they have all been found to improve fatigue for some people. Medications can be effective at improving some, but not all aspects of fatigue and are therefore helpful for some, but not all, people.
Amantadine is one of the more commonly used medications to treat MS fatigue. In small studies with short durations, amantadine was shown to be effective when compared with a placebo to help with fatigue. However, it’s important to note that these were very small studies. Another study compared amantadine with aspirin to decrease fatigue and both showed equal significant benefit. In this trial, there was no placebo group, so it will require further research to better characterize the role of these two drugs to help treat MS-related fatigue.
Provigil (modafinil) and Nuvigil (armodafinil) were developed to treat narcolepsy and excessive daytime sleepiness. Stimulant drugs, such as Ritalin and Adderal are commonly used to treat attention deficit disorders, and are sometimes used to treat MS fatigue. They can help with concentration and focus. Finally, Ampyra is a medication that helps to improves conduction in damaged nerve fibers. It can be very helpful in managing fatigue for a limited number of people. It has been shown to help with vision, walking, and cognition.
Many people have tried all of these medications and are still suffering with fatigue. There are no silver bullets.
Behavioral & Lifestyle Interventions
There are many ways to improve fatigue besides medications. Most of them, however, require an investment of time or energy or both, and when the problem is fatigue, both of those may be in short supply. The problem with most of them is that they are not immediate and it can take time to reap the benefits of changes you might make.

The best way to decrease fatigue is to increase your energy reserves. There are two ways to do that: make more energy, or use less. Sleep is probably the best and most overlooked treatment for fatigue and a good way to make more energy. Taking a nap can take care of immediate fatigue but some people find they can save up energy beforehand, by resting more before an event that may be more energy expensive. Evaluating and improving your sleep hygiene can help improve the quality of your sleep. More information on sleep hygiene strategies can be found in the article “Getting a Good Night’s Sleep,” from the Fall 2017 issue of InforMS, available at www.mscenter.org/informs.
It may be counter-intuitive, but one of the most effective treatments for fatigue is exercise. Exercise improves mood, decreases fatigue and improves quality of life. It can reduce pain and improve sleep. It decreases stress and anxiety. It improves self-efficacy and sense of control. It improves general health. Exercise helps make more energy. Multiple studies have demonstrated the positive impact that exercise has on reducing fatigue, increasing neurological reserve, and improving overall quality of life in people living with MS.
Energy conservation techniques are ways to think about spending less energy. Until forced to do so, many of us treat our energy supplies as if they were charge cards with no limits. We don’t think about how we use our energy and so we often don’t use it effectively. Fatigue management classes, often taught by occupational therapists, help people think about, organize and strategize what they want to do with their time and energy. Occupational therapists can also help people find easier, less energy expensive ways to complete home and work chores.
Energy conservation is also about identifying the things that waste your time, wear you out and drain your energy — and figuring out how to avoid them. That includes people, committees, movies you don’t like and things that take your energy and give you nothing back. For more information on energy conservation strategies, please read our interview with Occupational Therapist, Christy Dittmar on Page 15 of this issue.
Pay attention to your mood. Depression, mood disorders, fatigue and stress all hang out together. It is sometimes impossible to separate them. However, when people feel overwhelmed by fatigue, they are sometimes offended if you inquire about their mood. “I am tired, not crazy,” snapped one woman when she was queried about depression. Depression doesn’t always appear as depression, and in MS it can frequently present with primary symptoms of fatigue and irritability.
If your healthcare provider suggests treatments for depression as a starting point for treating fatigue, it does not mean that your reports of fatigue are not being taken seriously. Treatment for depression –either medication or cognitive behavioral therapy – can also improve fatigue. We have effective treatments for depression that really do work. Effectively managing mood disorders can give you more energy and create a greater sense of control and get you in a better place to think about what to do next.
Research studies have found that mindfulness meditation training improved the quality of life and decreased both fatigue and depression in people with MS. And meditation and relaxation training both help people manage stress. A 2018 review of research found that psychological interventions such as cognitive behavioral therapy, mindfulness-based therapy, and relaxation therapy were helpful strategies for treating MS fatigue.
From a dietary perspective, eliminating or reducing caffeine and alcohol can help improve your sleep and decrease your fatigue. Increasing your fruits and vegetables and decreasing your intake of sugars and refined carbohydrates can make a real difference in your energy levels.
For more information on nutrition and MS, please see the Fall 2017 issue of InforMS, featuring an interview with registered dietician Holly Prehn, and the Fall 2018 issue article “Fighting Fatigue with Healthy Eating Habits.” Both are available at our online archive, at www.mscenter.org/informs.
In the long run, behavioral interventions are probably more successful interventions to improve fatigue but they are harder to implement because they require change and it is hard to change.
Change requires energy and that can be in short supply when fatigue is the problem. It can be difficult to find the motivation to change, or to see the value of an investment that may have long-term benefits but has none for the short term.
When you are so fatigued you can’t move, it is hard to see the value of an exercise program, or of reorganizing the kitchen cupboard. It’s easier to take a pill or do nothing.
Change can also be difficult because for some people, to change means to give in to MS. To move the washing machine to the main floor, to get and use a handicapped parking permit, to take a nap – all these things can mean giving in to MS.
Making changes to manage fatigue is, to some extent, about giving in to MS. It’s about acknowledging that MS does create some real problems and impose some real restrictions. You can’t simply muscle your way through and pretend they don’t exist. It’s important to develop realistic expectations. It’s unlikely that you’ll discover a perfect solution. We often expect interventions to be as rapid and effective as penicillin is at treating strep throat, and that’s not the case with MS fatigue.
MS fatigue is a real and very complex problem. It takes time and thought to identify solutions that will work for you. Be patient with yourself, be persistent, and allow time for your strategies to begin to work.